Understanding Headaches: Causes, Care and a Real Case That Changed Everything
By Derrick Lian
Nearly 1 in 5 Australians live with recurring headaches or migraines-and they're not all the same. Some respond well to hands-on therapy, others need lifestyle changes, and in many cases, the key is knowing where the pain is really coming from.
Let's break down the common types-and share how one patient's breakthrough showed us just how powerful the right care can be.
The 3 Headaches We See Most Often
1. Tension-Type Headaches
These feel like a tight band across the forehead or back of the head-like your scalp or neck is "clenching." Common causes:
- Stress and emotional tension
- Long hours sitting at a desk
- Shallow breathing or jaw clenching
- Poor hydration and skipped meals
2. Cervicogenic Headaches
These start in the neck, often just below the skull, and radiate to the temple, forehead, or behind the eye-typically on one side.
Common triggers:
- Restricted upper cervical joints (C1-C3) Page 1 Understanding Headaches
- Postural fatigue (desk, phone use)
- Old whiplash or neck injuries
- Poor neck rotation or movement patterns
3. Migraine Headaches
Throbbing, often one-sided, sometimes behind the eye or temple. Can come with nausea, light/sound sensitivity, or visual aura.
Typical triggers:
- Hormonal changes (especially in women)
- Neck tension and poor sleep
- Food sensitivities or alcohol
- Dehydration or skipped meals
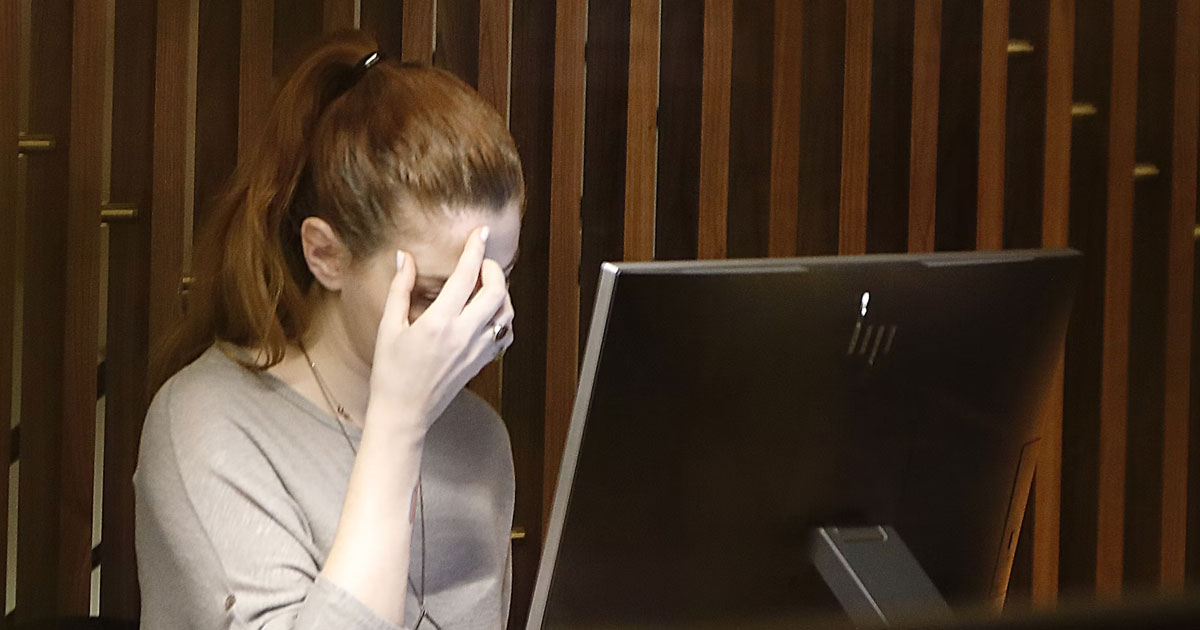
A Real Case: Beth's Headache Journey
Beth, a 34-year-old project manager, came to our clinic with daily headaches that had persisted for nearly two years.
Symptoms:
- Dull ache behind her right eye
- Worsened by screen time, meetings, and stress
- Peak intensity mid-afternoon, every day
- OTC painkillers gave only brief relief
- Previously misattributed to "sinus pressure" or "maybe migraines"
What We Found:
Beth had stiffness at C1/C2, hypertonic suboccipitals and right SCM, and weak deep neck flexors. Posture showed significant forward head carriage.
Treatment Plan:
- Gentle cervical joint mobilisation
- Targeted soft tissue release (suboccipitals, SCM)
- Postural retraining and ergonomic coaching
- Breathing and hydration strategies
After 4 sessions, Beth's headaches dropped from daily to 1-2x/week. By week 3, she had her first headache-free week in years. At her 3-month review, she'd gone 6 weeks without a single episode.
Why It Worked
Not all headaches come from the neck-but when they do, treating the neck is the key. In Beth's case, the missing piece wasn't another scan or medication-it was recognising the mechanical root cause and restoring proper function.
When Should You See a Chiropractor for Headaches?
- Headaches worsen with neck movement or posture
- Pain is one-sided or behind the eye
- You feel pressure at the base of the skull
- You've tried medications but still suffer
- You want to manage the root cause, not just mask symptoms
You don't have to live with recurring headaches. With the right assessment and tailored care plan, it's often possible to find long-term relief-drug-free and rooted in understanding your body, not fighting it.