10 Facts About Frozen Shoulder
1. The medical name for frozen shoulder is “Adhesive Capsulitis”.
2. Frozen shoulder is a painful condition which involves progressive restriction of shoulder movements.
Those afflicted by frozen shoulder often experience difficulty and pain in dressing and overhead activities. Commonly, people also continual pain which disturbs sleep at night.
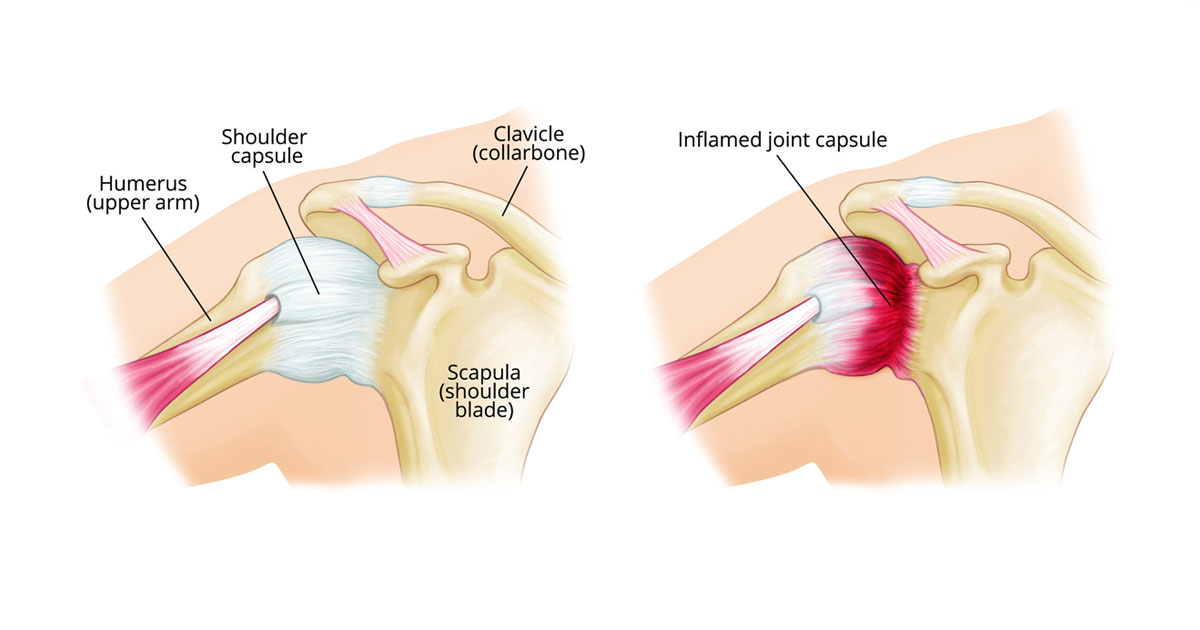
3. Restricted and painful movement is caused by the connective tissue encapsulating the shoulder joint tightening and becoming inflamed.
4. The actual mechanism or trigger of frozen shoulder is unknown.
Accordingly, majority of frozen shoulder cases occur without any clear reason why, but a portion will develop frozen shoulder after trauma or injury to the shoulder.
5. Frozen shoulder affects 3-5% of adults, commonly between 40-60years old(1).
It is also four times more common in women than men(2).
6. A person has significantly increased risk of developing frozen shoulder if you have a history of systemic disease Systemic disease includes conditions such as diabetes, hypothyroidism or cardiovascular disease(1).

7. The average duration of a frozen shoulder is between 1-3years(1). Historically, frozen shoulder was thought to be “self-limiting”, i.e. a condition that resolves after a given time by itself. However, emerging evidence is finding this to be a false assumption(3,4), and unfortunately in some people symptoms can last up to 10years(1).
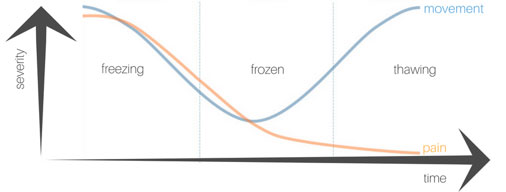
8. Frozen shoulder progresses through 3 distinct stages: freezing, frozen, thawing.
1) Freezing stage:
Gradual development of un-easing shoulder pain which becomes sharp at end-range movements. People will often experience pain at night, both sleeping on and off shoulder, which disturbs sleep. In this stage, range of movement is still largely preserved.
2) Frozen stage:
Resting shoulder pain begins to slowly subside with sharp pain only experienced at end-ranges of movement. Concurrently, the shoulder becomes progressively stiffer, and a person’s range of movement is significantly reduced
3) Thawing stage:
The final stage in which there is gradual improvement in shoulder range of movement with resolution of pain.
9. In the “freezing” stage, your General Practitioner or Physiotherapist may recommend to have cortisone steroid injections into the shoulder joint.
This is because they have been showed to be very effective at reducing pain in the early stages of frozen shoulder(5). However, they do not improve range or speed up resolution of frozen shoulder.
10. In the “thawing” stage, Physiotherapy-guided rehabilitation will be beneficial to facilitate restoration of shoulder function.
Aim of treatment which be to regain range of motion at the shoulder and correct any altered movement patterns

References:
1. Manske, R. C., & Prohaska, D. (2008). Diagnosis and management of adhesive capsulitis. Current reviews in musculoskeletal medicine, 1(3-4), 180–189. doi:10.1007/s12178-008-9031-6
2. Mezian K, Chang KV. Frozen Shoulder. [Updated 2019 Feb 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482162/
3. Wong CK, Levine WN, Deo K, Kesting RS, Mercer EA, Schram GA, Strang BL. Natural history of frozen shoulder: fact or fiction? A systematic review. Physiotherapy. 2017 Mar;103(1):40-47. doi: 10.1016/j.physio.2016.05.009. Epub 2016 Jun 21. Review. PubMed PMID: 27641499.
4. Vastamäki H, Kettunen J, Vastamäki M. The natural history of idiopathic frozen shoulder: a 2- to 27-year followup study. Clin Orthop Relat Res. 2012 Apr;470(4):1133-43. doi: 10.1007/s11999-011-2176-4. Epub 2011 Nov 17. PubMed PMID: 22090356; PubMed Central PMCID: PMC3293960.
5. Page MJ, Green S, Kramer S, Johnston RV, McBain B, Chau M, Buchbinder R. Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. 2014 Aug 26;(8):CD011275. doi: 10.1002/14651858.CD011275. Review. PubMed PMID: 25157702.